Medical Practice Hygiene Checklist: The Ultimate Guide for Optimal Practice Hygiene
Discover the ultimate medical practice hygiene checklist with practical tips for daily routine, cleaning schedules, data protection, and hygiene inspections. Optimize your practice organization efficiently.
Inhaltsverzeichnis
Medical Practice Hygiene Checklist: The Ultimate Guide for Optimal Practice Hygiene
Why a Systematic Medical Practice Hygiene Checklist is Indispensable
A professional medical practice hygiene checklist forms the foundation for patient safety and legally secure practice management. Strict hygiene regulations apply in medical practices, and compliance has both medical and legal consequences. Systematic documentation and implementation of hygiene measures is not only legally required but also protects against costly legal disputes and reputation damage.
Infection protection laws and hygiene regulations require every medical practice to comply with specific hygiene standards. A systematic practice checklist helps to fully meet all legal requirements. Official guidelines form the basis for implementing recommendations, while medical device regulations govern the proper preparation of medical instruments. Occupational health and safety laws ensure protection of staff and patients from infection risks, and technical rules define standards for biological working materials in healthcare.
Inadequate hygiene measures can have serious consequences. A daily practice checklist significantly minimizes these risks by ensuring structured processes. For patients, poor hygiene creates risks such as healthcare-associated infections through cross-contamination, transmission of resistant germs, and prolonged healing processes and complications. For the practice itself, liability claims and compensation demands, reputation damage and patient loss, regulatory sanctions up to practice closure, and increased insurance premiums can result.
A well-thought-out checklist in the medical practice optimizes workflows and reduces costs long-term through various mechanisms. Standardized procedures significantly shorten cleaning times, while clear responsibilities reduce search time and efficient documentation prevents duplicate work. Preventive measures prevent expensive follow-up treatments, optimize disinfectant consumption, and reduce downtime through systematic maintenance.
Daily Medical Practice Checklist: The Most Important Hygiene Measures at a Glance
A structured daily practice checklist ensures that all critical hygiene points are systematically addressed. This routine equally protects patients and staff from infection risks and ensures smooth practice operations.
Hygiene Before Treatment Begins
The morning routine before the first patient forms the foundation for a hygienically impeccable practice day. Systematic completion of the following points ensures optimal starting conditions:
- Hand hygiene: Hygienic hand disinfection by all staff
- Surface disinfection: Treatment tables, work surfaces, and handles
- Instrument check: Verify sterility and functionality
- Disinfectant: Check fill levels and refill
- Personal protective equipment: Availability of gloves, masks, gowns
- Air quality: Activate ventilation, check room temperature
- Documentation: Begin hygiene protocol for the day
Special areas require particular attention: In the preparation room, functionality of sterilizers is checked, while in the waiting room, seating surfaces and magazines are disinfected. Restrooms are checked for proper functioning of soap dispensers and towel machines.
Between Patients: Disinfection and Cleaning
Intermediate disinfection after each patient is carried out systematically and completely:
- Hand disinfection: Before and after each patient contact
- Surface disinfection: All patient-near surfaces
- Instrument change: Properly dispose of used instruments
- Glove change: Change disposable gloves after each patient
- Waste disposal: Properly dispose of contaminated materials
Special attention is given to situations involving blood or body fluid contact, infectious patients requiring isolation, and invasive procedures or injections that necessitate increased hygiene measures.
End of Practice Day: Closing Routine
The daily closing requires systematic completion of all important hygiene points:
- Final disinfection: Large-scale disinfection of all rooms
- Instrument preparation: Cleaning, disinfection, sterilization
- Waste disposal: Complete disposal of all waste categories
- Equipment cleaning: Medical devices according to manufacturer specifications
- Documentation: Complete recording of all measures
- Material check: Check consumables for the next day
- Room cleaning: Mop floors, empty trash cans
Weekly additional tasks supplement the daily routine: Refrigerator temperatures are documented, sterilizer maintenance follows the protocol, and emergency equipment is checked.
Medical Practice Cleaning Schedule Checklist: Developing Structured Cleaning Routines
A professional cleaning schedule checklist ensures systematic and traceable cleaning of all practice areas. The structured approach not only meets hygiene standards but also optimizes workflows and resource utilization.
Daily Necessary Cleaning Work
High-frequency cleaning areas require special attention and systematic processing. In treatment rooms, after each patient, treatment tables are disinfected with approved agents, followed by wipe disinfection of all contact surfaces and work surfaces. Door handles and light switches are disinfected as frequently touched surfaces, while medical equipment receives surface cleaning according to manufacturer specifications. Visible floor contamination is immediately removed to maintain hygiene.
The waiting room and reception are cleaned multiple times daily, with seating surfaces disinfected between patient groups and toys disinfected after use. Magazines are regularly exchanged and disinfected, while counters and reception receive regular surface disinfection.
Restroom areas receive intensive cleaning at least three times daily: Toilets are completely cleaned and disinfected, wash basins including taps and shelves are thoroughly processed. Soap dispensers are refilled and cleaned externally, towel dispensers undergo function checks and refilling. Floors are wet-cleaned and treated with disinfectant additive.
Weekly and Monthly Deep Cleaning
Weekly cleaning work follows a structured schedule for optimal results. In treatment areas, intensive floor cleaning of all treatment rooms occurs Monday, windows and glass surfaces are cleaned Tuesday, while ventilation slots and air conditioning filters are checked Wednesday. Cabinets and shelves inside and out are due for cleaning Thursday, Friday handles equipment intensive cleaning and calibration.
Common areas also receive weekly attention: In the kitchen or break room, refrigerator, microwave, and coffee machine are cleaned, staff areas like changing rooms and break rooms are thoroughly processed. Storage rooms undergo inventory checks and organization.
Monthly special cleaning is systematically distributed over four weeks. In the first week of the month, complete maintenance and calibration of sterilizers occurs along with autoclave cleaning with descaling according to manufacturer specifications. Water lines are flushed and Legionella prevention carried out.
The second week focuses on lighting with cleaning of lamps and reflectors and dusting and cleaning of ceilings and high surfaces. Fire protection equipment undergoes function testing.
In the third week, upholstered furniture is due for professional cleaning or replacement, carpets and floor coverings receive basic cleaning, and window frames and door frames are intensively cleaned.
The fourth week includes cleaning of IT equipment such as keyboards, monitors, and printers, complete inspection of emergency equipment, and dusting and organization in archive rooms.
Documentation and Tracking of the Cleaning Schedule
Digital documentation systems revolutionize management of a modern checklist in the medical practice. Digital recording enables automatic reminders, compliance verification, quality assurance, and efficiency increases through optimized workflows.
Documentation requirements include time-accurate recording of date and time of each cleaning process and clear assignment of responsibility to the performing person. Disinfectants used and their concentration are documented, while special occurrences, deviations, and problems are noted. Follow-up checks ensure quality assurance through systematic spot checks.
Quality control occurs in multiple stages: Weekly spot checks by practice management monitor ongoing quality, while monthly evaluations of cleaning quality show trends. Quarterly training of cleaning staff keeps knowledge current, supplemented by annual review and adjustment of the entire cleaning schedule.
Data Protection Medical Practice Checklist: Making Hygiene Documentation Legally Secure
A data protection medical practice checklist for hygiene documentation must meet both medical compliance and GDPR requirements. Legally secure documentation protects against regulatory sanctions and liability risks.
GDPR-Compliant Documentation of Hygiene Measures
Data minimization and purpose limitation require that hygiene documentation may only contain actually necessary data. Permitted are timestamps with date and time of hygiene measures, the performing person via employee ID or initials without full names, and the type of measure such as cleaning, disinfection, or sterilization. Products used are documented with product name and concentration, affected areas are recorded as room or device without patient reference, and control results are noted with measured values and test results.
Prohibited, however, are patient names in hygiene documents, detailed treatment information, unnecessary personnel data, and biometric data without appropriate legal basis.
Technical and organizational measures (TOM) ensure data security: Digital hygiene documents are stored encrypted, role-based permissions are implemented, and all access and changes are logged. Secure and encrypted data backup and automatic deletion after retention periods complete the security concept.
Retention Periods and Archiving
Legal retention periods distinguish between short and long-term documentation. Daily hygiene checklists and temperature documentation must be retained for two years, intermediate disinfection protocols and consumable records for one year. Sterilization protocols require five years retention after last use, while maintenance documentation, hygiene inspection protocols, and training records must be archived for ten years.
Analog archiving occurs in fireproof filing cabinets with systematic organization by year and access control. Digital archiving uses unalterable PDF documents with digital signature, redundant storage, and regular migration to current data carriers.
Digital vs. Analog Documentation Systems
Digital systems offer considerable advantages: automatic reminders, instant document availability, automatic evaluations, and reduced paper consumption. Legal security is ensured through automatic backups, unalterable timestamps, and audit trails. Quality assurance occurs through standardized input masks, plausibility checks, and trend analyses.
Analog systems have disadvantages such as high manual effort, error-proneness, and difficult archiving. A hybrid approach combines digital main documentation with analog emergency backups and enables mobile recording and cloud synchronization with offline capability.
Opening a Medical Practice Checklist: Hygiene Requirements from the Start
When opening a practice, a well-thought-out opening a medical practice checklist for hygiene requirements is essential. Early planning prevents costly modifications and ensures the highest standards from the beginning.
Structural Requirements for Optimal Hygiene
Floor plan design with hygiene orientation defines clear functional areas: clean areas like treatment rooms and sterilization, unclean areas for preparation and waste, and neutral areas like reception and waiting room. Traffic flow follows the one-way principle for contaminated materials with separate access and short paths between treatment and preparation.
Surface materials include seamless, disinfectant-resistant floor coverings, washable wall cladding up to two meters height, and smooth, cleaning-friendly ceilings. Supply and disposal require sufficient wash basins with single-lever mixers, separate waste water disposal, controlled room air technology, and RCD-protected power connections.
Initial Equipment and Hygiene Devices
Basic equipment for a hygienically impeccable practice includes various areas:
Hand hygiene stations:
- Wash basins (at least 1 per treatment room)
- Disinfectant dispensers with sensor
- Touchless single-use towel dispensers
Sterilization and preparation:
- Autoclave appropriate to practice size
- Washer-disinfector (WD)
- Ultrasonic bath for gentle pre-cleaning
- Sealing device for sterile packaging
Personal protective equipment:
- Disposable gloves in various sizes
- FFP2/FFP3 and surgical masks
- Long-sleeved, water-repellent gowns
- Safety glasses for splash protection
Official Approvals and Certifications
Registrations and approvals from various authorities require specific documentation:
Health Department:
- Detailed hygiene concept
- Evidence of staff training
- Waste concept with disposal contracts
- Drinking water testing (Legionella test)
Medical Association:
- License to practice for treating physicians
- Specialist training certification
- Quality management system
Health Insurance Association:
- Application for insurance authorization
- Hygiene inspection before authorization
- Contracts with certified laboratories
- Evidence of required emergency equipment
Documentation requirements before opening include detailed hygiene plans for all areas and systematic staff training. Early implementation of a medical practice hygiene checklist creates the foundation for legally secure practice management.


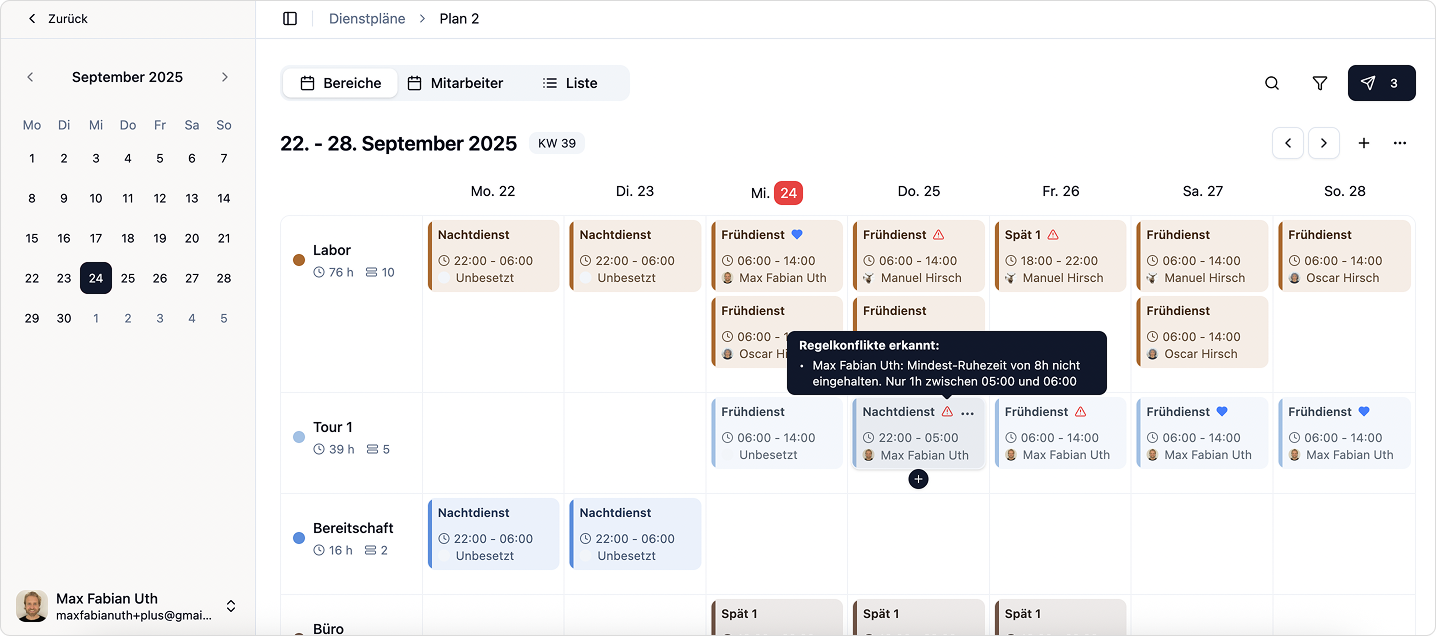
Try Medishift for free now!
- Modern duty planning in just minutes
- Automated workflows for your practice
- Forever free for up to 10 employees
Hygiene Inspection Checklist Medical Practice: Perfectly Prepared for Inspections
A comprehensive hygiene inspection checklist for medical practices optimally prepares for official inspections and minimizes risk of complaints. Preventive self-monitoring includes preparing current hygiene plans, training records, maintenance protocols, and temperature logs. Spatial preparation occurs through complete cleaning of treatment rooms, orderly instrument sorting, and correct waste separation.
Typical inspection points by health authorities focus on hand hygiene with sufficient wash basins and approved disinfectants, surface hygiene with documented cleaning schedules, instrument preparation with proper sterilization, and waste management with correct categorization.
For complaints, immediate measures address safety risks and documentation gaps, medium-term improvements handle structural deficiencies, and long-term strategies address practice modernization. Systematic application as a permanent quality assurance instrument ensures compliance and continuously improves patient care.
Digital Solutions for an Efficient Checklist in the Medical Practice
Modern digital solutions are revolutionizing hygiene organization in medical practices. A professional checklist in the medical practice as a digital application optimizes workflows, increases compliance, and significantly reduces administrative burdens.
Advantages of Digital Checklist Apps
Digital solutions offer decisive improvements over analog systems:
Efficiency increase:
- Automatic reminders for due hygiene measures
- Pre-filled forms for recurring data
- Offline functionality for uninterrupted work
Quality assurance:
- Completeness checks prevent incomplete documentation
- Consistent standards through uniform execution
- Automatic plausibility checks reduce errors
Legal security:
- GDPR-compliant documentation with encrypted data storage
- Role-based access control for data protection
- Unalterable timestamps and audit trails
Integration with existing practice software enables seamless connection with practice management systems, medical devices, and QM systems. Cloud-based architecture offers multi-device synchronization and automatic backups.
medishift is a digital solution that makes it very easy to capture checklists, document them, and efficiently deliver them to employees. The app offers fully digitized hygiene documentation with an intuitive user interface and automatic compliance checks. As a central platform, medishift enables seamless distribution of hygiene checklists to the entire practice team while ensuring complete documentation of all hygiene measures. The implementation strategy includes gradual migration, staff training, and continuous optimization. Digitalization transforms hygiene processes into efficient, quality-assuring routines for patients and staff.


